
Constipation and diarrhoea: what is the connection?
We all experience constipation or diarrhoea from time to time. That’s a fact, even if social conventions mean tummy troubles might not be in the top tier of conversation topics when we hang out with our friends. While bowel movements tend to be something we keep private in most cases, they play an integral role in maintaining healthy, full lives.
Constipation and diarrhoea may be at opposite ends of the bowel movement spectrum but is there a connection between the two?
In this article we discuss the definitions of both constipation and diarrhoea, the possible associations between the two, and how to best manage them.
Constipation
Constipation can leave you feeling very bunged up, causing severe levels of discomfort that you might be embarrassed to talk about. But there's nothing shameful about it. It’s estimated that 15% of the global population experiences constipation, and the medical community is always searching for new ways to help you manage it.1
Normal pooping patterns are challenging to define. The frequency of bowel movements in most people ranges from one stool every three days, to three stools per day2, which is a pretty wide range! As a general rule, if you go less than three times per week, you could be constipated, but bowel movements vary widely between individuals, as well as the subjective perception of what constitutes “normal”.
Symptoms of constipation include abdominal pain, bloating, flatulence, nausea, and even headaches and fatigue.2 Health professionals use standardised diagnostic criteria to diagnose all types of illnesses and conditions.1 Rome’s IV is the diagnostic tool that defines constipation. Two of six signs and symptoms must be present for a doctor to diagnose constipation. The six signs and symptoms are:1
- straining
- hard stools
- incomplete evacuation
- manual manoeuvres to assist or support defecation
- blockage sensations
- less than three bowel movements per week.
What causes constipation?
Getting to the root cause of your constipation isn't always easy. That's because there are so many things that have the potential to lead to a blockage or slowing down of your bowel movements.
Several factors can trigger constipation, including:
- an unbalanced diet
- a lack of fibre
- dehydration
- a sedentary lifestyle
- medical conditions
- fasting
- stress
- medication side effects
With its increasingly hectic pace, modern life may also increase our risk of adopting these unhealthy habits, which can in turn negatively affect our digestive systems as well.4
So, this leads us to the important question; is constipation manageable? The answer, thankfully, is yes.
Let’s explore a few options.
Managing constipation
The following are some ways in which people can manage their constipation:
People should know that "normal" bowel movements vary from person to person. The key is monitoring yourself, and adjusting your habits accordingly so that you are comfortable.3
It is essential to be aware that lifestyle changes are likely to be necessary. Monitoring your progress and establishing a regular bowel routine is important.
Make sure you exercise regularly, as research shows exercise can get your bowels moving as well.4
Most constipation treatments begin with dietary changes. Increase your fibre intake, drink water, for starters.5
If these do not provide relief, there are alternatives, such as laxatives.
See our full range of Dulcolax products here, including tablets, suppositories and liquid.
Diarrhoea
Diarrhoea refers to a condition in which stool weighs more than 7 ounces per day. A patient with diarrhoea will generally describe stool that is too abundant, too frequent, too soft, urgent, and challenging to retain.6
Acute diarrhoea is diarrhoea that lasts less than two weeks. A persistent diarrhoeal illness usually lasts between two and four weeks. It is considered chronic diarrhoea when it persists for more than four weeks.7
What causes diarrhoea?
Multiple factors can lead to acute diarrhoea, so determining the cause is crucial. Here are the more common ones:
Viruses: In most cases, acute, watery diarrhoea is caused by viruses (viral gastroenteritis). In children, rotavirus is the most common one, followed by norovirus in adults.
Lactose, sorbitol and fructose intolerance: People who are intolerant may experience watery diarrhoea if they consume soft drinks, juices, dried fruits, or gums containing these ingredients.
Some medications: Antibiotics commonly cause Diarrhoea as a side effect. In addition, some other medications have side effects that can cause diarrhoea, including non-steroidal anti-inflammatory drugs (NSAIDs), antacids, antihypertensives, antibiotics, and antiarrhythmics.
Chronic diarrhoea also has multiple causes, which includes coeliac and Crohn’s disease, parasitic intestinal infections, irritable bowel syndrome. If you're experiencing chronic diarrhoea, it's important to speak to your doctor.7
Managing diarrhoea
Acute diarrhoea usually resolves with simple dietary changes. You should consult a doctor if you feel ill, have bloody diarrhoea, intense abdominal pain, or have diarrhoea that persists for more than 48 hours.
You may need blood tests if you have severe diarrhoea to determine if you need to replace fluids, electrolytes, and minerals, such as magnesium, potassium, and zinc.
Your doctor will order several tests if you have chronic diarrhoea to determine the cause and possible complications.7
How constipation can cause diarrhoea
What does it mean to be constipated and then have diarrhoea? While it may seem counterintuitive, it’s possible to have diarrhoea after constipation. If you’re suffering from constipation then diarrhoea, here are some possible causes.
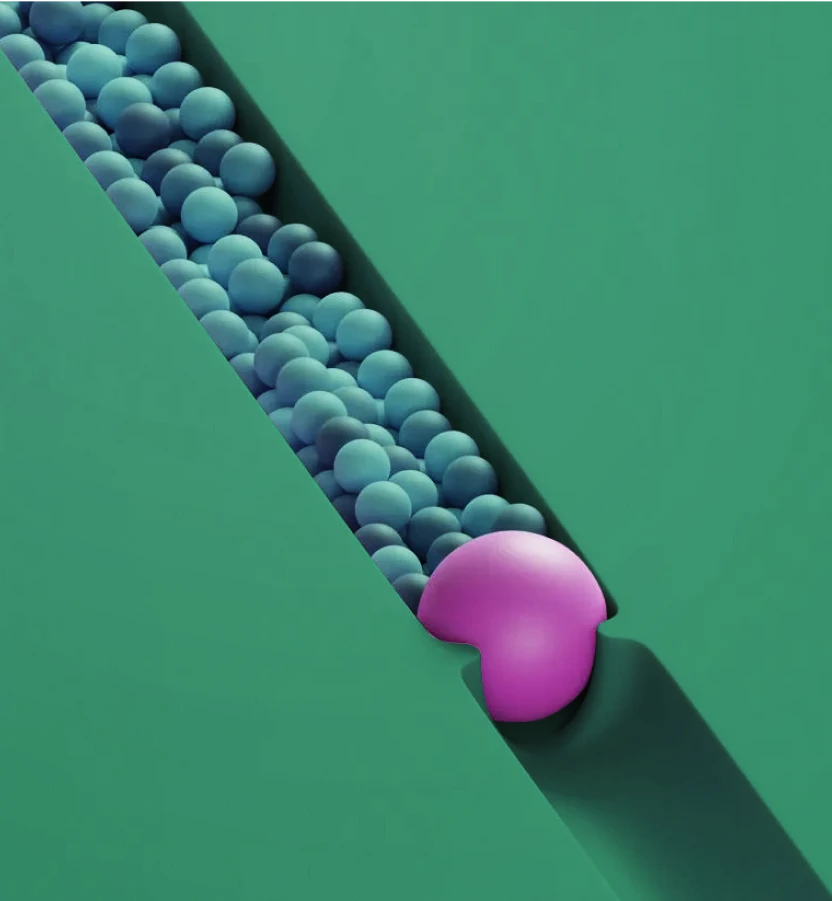
Overflow diarrhoea can be triggered by severe constipation because the internal anal sphincter relaxes, allowing the stool contents to pass through. Patients often describe their symptoms as diarrhoeal due to the appearance of liquid stool.8
Overflow diarrhoea, also known as paradoxical diarrhoea, occurs when stool seeps from around an intestinal impaction. Chronic constipation is typically associated with this condition.9
Several conditions, including irritable bowel syndrome (IBS), can manifest with alternating diarrhoea and constipation, making it critical to see your GP for a complete diagnosis.10
How to prevent overflow diarrhoea
When to see a doctor or pharmacist about constipation and diarrhoea
First off, remember that you’re not alone. Diarrhoea and constipation are conditions that can affect anyone and you should not feel embarrassed to discuss them with your doctor or pharmacist. Several safe and effective protocols exist for the management of both diarrhoea and constipation.
See a full range of Dulcolax products here, including tablets, suppositories and liquid.
Monitor your bowel movements for any unusual changes and take a proactive approach to caring for your digestive system, so that you can participate in all life has to offer with greater energy and enthusiasm.
Sources
- Rao, S.S. (2022). Approach to the patient with constipation. In Yamada's Textbook of Gastroenterology (eds T.C. Wang, M. Camilleri, B. Lebwohl, A.S. Lok, W.J. Sandborn, K.K. Wang and G.D. Wu). https://doi.org/10.1002/9781119600206.ch36
- Poitras, P., Bouin, M., Faure, C., Dapoigny, M. (2022). Constipation. In: Poitras, P., Bilodeau, M., Bouin, M., Ghia, JE. (eds) The Digestive System: From Basic Sciences to Clinical Practice. Springer, Cham. https://doi.org/10.1007/978-3-030-98381-9_15
- Rao, Satish S.C. MD, PhD1; Lacy, Brian E. MD, PhD2; Emmanuel, Anton MD3; Müller-Lissner, Stefan MD4; Pohl, Daniel MD5; Quigley, Eamonn M.M. MD6; Whorwell, Peter MD, PhD7. Recognizing and Defining Occasional Constipation: Expert Consensus Recommendations. The American Journal of Gastroenterology: November 2022 - Volume 117 - Issue 11 - p 1753-1758 doi: 10.14309/ajg.0000000000001945
- Camilleri, M., Ford, A., Mawe, G. et al. Chronic constipation. Nat Rev Dis Primers 3, 17095 (2017). https://doi.org/10.1038/nrdp.2017.95
- Portalatin M, Winstead N. Medical management of constipation. Clin Colon Rectal Surg. 2012 Mar;25(1):12-9. doi: 10.1055/s-0032-1301754. PMID: 23449608; PMCID: PMC3348737.
- Poitras, P. (2022). Diarrhea. In: Poitras, P., Bilodeau, M., Bouin, M., Ghia, JE. (eds) The Digestive System: From Basic Sciences to Clinical Practice. Springer, Cham. https://doi.org/10.1007/978-3-030-98381-9_13
- Ochoa, B. and Surawicz, C.M. (2012) Diarrheal Diseases – acute and chronic, American College of Gastroenterology. American College of Gastroenterology. Available at: https://gi.org/topics/diarrhea-acute-and-chronic/ (Accessed: December 6, 2022).
- Hecht, G.A. and Trieu, J.A. (2022). Approach to the patient with diarrhea. In Yamada's Textbook of Gastroenterology (eds T.C. Wang, M. Camilleri, B. Lebwohl, A.S. Lok, W.J. Sandborn, K.K. Wang and G.D. Wu). https://doi.org/10.1002/9781119600206.ch35
- Van, Jeremy DO; Abraham, Rana MS, MD. 1550 Overflow Diarrhea in the Setting of Urinary Retention. The American Journal of Gastroenterology: October 2019 - Volume 114 - Issue - p S860-S861 doi: 10.14309/01.ajg.0000595728.24592.62
- Woods TA. Diarrhea. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 88. Available from: https://www.ncbi.nlm.nih.gov/books/NBK414/
- Kim, D.W. and Seres, D.S. (2022). Nutrition Support. In Yamada's Textbook of Gastroenterology (eds T.C. Wang, M. Camilleri, B. Lebwohl, A.S. Lok, W.J. Sandborn, K.K. Wang and G.D. Wu). https://doi.org/10.1002/9781119600206.ch23
- D’Aoust, L., Poitras, P. (2022). Diets and Digestive Diseases. In: Poitras, P., Bilodeau, M., Bouin, M., Ghia, JE. (eds) The Digestive System: From Basic Sciences to Clinical Practice. Springer, Cham. https://doi.org/10.1007/978-3-030-98381-9_29
- Kim YS, Song BK, Oh JS, Woo SS. Aerobic exercise improves gastrointestinal motility in psychiatric inpatients. World J Gastroenterol. 2014 Aug 14;20(30):10577-84. doi: 10.3748/wjg.v20.i30.10577. PMID: 25132778; PMCID: PMC4130869.
- Araghizadeh F. Fecal impaction. Clin Colon Rectal Surg. 2005 May;18(2):116-9. doi: 10.1055/s-2005-870893. PMID: 20011351; PMCID: PMC2780143.





.webp)
